Every day, 50 women will be diagnosed with breast cancer in Australia. In addition, three men in Australia will also be diagnosed with breast cancer each week.

Pioneering professor: John Boyages has more than 30 years of experience in the diagnosis and treatment of breast cancer.
As I look back over my last 35 years of diagnosing and treating patients with breast cancer, I find it amazing to see the number of changes and innovations in treatment that were simply not available previously.
When I was a medical student, patients with a breast lump would wake up after an anaesthetic not even knowing if they had had a mastectomy (total removal of the breast) or not.
Most patients diagnosed with breast cancer naturally want something done immediately. The reality is that the cancer has probably been present for many months, if not years, and taking an extra week or so to work out exactly what is going on can be vitally important.
Tailored treatment
Today, most patients do not need a mastectomy and removal of all the lymph nodes under the armpit is less common.
There are many patients whose disease cannot be seen easily on a mammogram - a screening tool to detect early breast cancer - and this is where a breast MRI is important.
Further, for some patients with more aggressive tumours known as “HER2 positive” or “triple-negative” tumours, having a preoperative PET/CT scan can determine a treatment strategy that may be totally different to one based on conventional imaging.
For some patients, we now give chemotherapy first to shrink the tumour, rather than surgery. This is known as “neoadjuvant chemotherapy”.

Future hope: The chance of surviving breast cancer is increasing thanks to medical advances.
We then repeat the PET or other scans after chemotherapy to help determine a personalised care plan that may mean less surgery with fewer complications and an increased chance of saving the breast.
Although several trials are ongoing in this area, many institutions around the world have started to "de-escalate" therapy. This means doing fewer axillary dissections (a surgical procedure to remove lymph nodes) but continuing to do a sentinel lymph node biopsy and tailored radiation therapy to reduce the incidence of complications such as lymphoedema - a lifelong progressive condition, often beginning with slight swelling which gradually escalates.
Macquarie University is leading the way through its Genesis Cancer Care Radiation Therapy Department by using a technique where patients take a deep breath during treatment, and hold this breath while "VMAT" (volumetric modulated arc therapy) radiation is delivered (see image below).
This sophisticated radiation technique can reduce the amount of lung and heart that need to be treated, leading to fewer complications in the future.
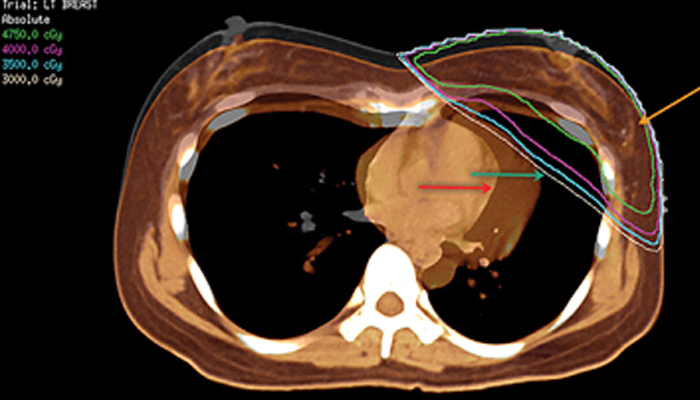
A fused image showing the heart covered by a radiation beam (normal breathing, green arrow) and missed after deep inspiration (orange arrow); breast cancer location marked at surgery by titanium clips after its removal (orange arrow).
Survival rates can be increased by up to 10% using VMAT, because we can easily treat the lymph nodes behind the breast bone (called the internal mammary chain). Many centres simply ignore this area, despite international guidelines proving the survival benefit of radiation therapy.
The Macquarie Breast Cancer Program has a multi-disciplinary team that meets regularly and discusses patients both preoperatively and postoperatively, supported not only by surgeons, radiation oncologists and medical oncologists but also by psychologists, occupational therapists, breast care nursing and even a medical librarian.
- New breast health clinic the first of its kind in Australia
- Will we ever cure cancer?
- Many advanced melanomas can now be beaten
Sponsored in part by the McGrath Foundation, a new McGrath breast care nurse will also be starting soon at Macquarie University Hospital.
The ALERT (Australian Lymphoedema Education Research and Treatment) program works closely with the breast program and offers preoperative and postoperative assessment and lymphoedema checks. It is the only centre in Australia offering a multidisciplinary care approach to this condition, with advanced diagnostic imaging and several surgical treatments for this condition, which can be psychologically and physically crippling.
Meanwhile, Professor Hiroo Suami and I have been invited to the second Harvard Symposium on Lymphoedema where we will be presenting five lectures and one workshop, including my presentation to a public forum on "Breast Cancer: Taking Control after Treatment" for Breast Cancer Month.
We have also been invited to Memorial Sloane Kettering Cancer Centre in New York to meet their Lymphoedema Task Force.
- Professor Boyages' books are available from bcpublish.com at a 40% discount using the coupon code, ALERT for the month of October - Breast Cancer Awareness Month.



