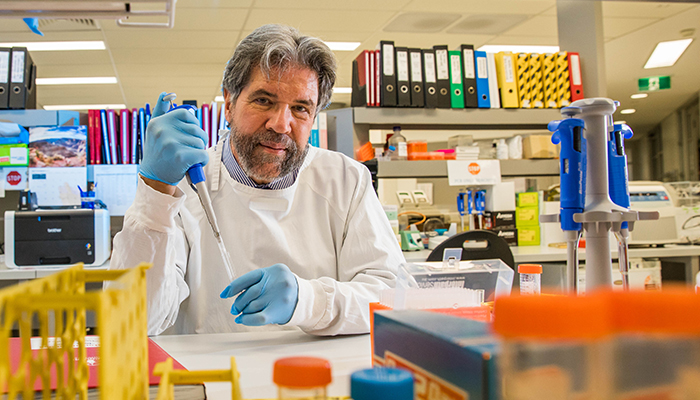
New treatments are beating advanced melanomas, says Professor Rick Kefford.
A cure for advanced melanoma is Professor Rick Kefford’s holy grail. After three decades immersed in cancer research, running more than 50 clinical trials, writing hundreds of journal articles and saving thousands of lives – that goal now seems to be within his reach.
“I do look back sometimes on some of the young patients that I looked after five years ago who died. I know, had they presented just three years later, we would have had an excellent chance of saving them,” he says. “That’s the heartbreak.”
Despite the poignant losses, Kefford believes that the tide is turning, and that many advanced melanomas can now be beaten.
“It’s an extraordinary time to be working in cancer research because the progress for nearly all of human cancer is exponential,” he says.
“Some of the world’s brightest young doctors and medical researchers come here to work with us, because of the nature of the research and our involvement in the very latest ground-breaking clinical trials.”
Australia has the world’s highest rate of melanoma. The skin cancer is Australia’s third most common cancer, and it is the most common cause of cancer death in young Australian adults aged 18 to 39.
Kefford heads Macquarie University’s Department of Clinical Medicine and is Co-Director of Research at Melanoma Institute Australia.
Since 2006, he has led a large NHMRC-funded research program involving a team of more than 100 scientists and doctors investigating melanoma susceptibility, prognosis and treatment.
An end to chemotherapy
Most melanoma is cured by surgery, but in about 20 per cent of cases the cancer spreads ('metastasises') before surgery is possible and goes on to cause about 2000 deaths each year in Australia – more than the national road toll.
But Kefford says that a revolution in treatment of metastatic melanoma has occurred over the past five years and about half the patients with the condition will now survive much, much longer.
Much of the breakthrough in cancer treatment is due to a new class of drugs called immune checkpoint inhibitors, which convince a patient’s own immune system to attack and kill the melanoma cells.
Three of them, ipilimumab, nivolumab and pembrolizumab are now reimbursed on the Australian Pharmaceutical Benefits Scheme.
Pioneering clinical trials of these drugs, in which Kefford played a leading role, helped fast-track their approval in the US and Australia by 2016.
“We are now pretty confident that if the disease completely disappears on these drugs and then the patient is disease-free three to six months after we stop treatment, that they will remain disease-free, or effectively cured.
“But it’s still very early days to claim a cure, because we don't know whether these patients are going to relapse somewhere down the track,” he cautioned.
Ten years ago, chemotherapy was the primary weapon against metastatic melanoma, but now it’s rarely used in melanoma treatment, says Kefford.
Patients would become very ill and sometimes die from chemotherapy side-effects but, while new drugs also have side-effects, Kefford says these are far more tolerable – and far less cruel.
“Chemo is in some ways a primitive, almost medieval, blunderbuss form of cancer treatment – but it is still terribly useful in some areas where we don't yet have better weapons.”
Precision cancer treatment
Kefford’s current research, with Professor Helen Rizos and the team at the Macquarie Precision Cancer Therapy Laboratory, uses the extensive Melanoma Institute Australia Research Database, which links melanoma bio-samples with detailed data about the patient, their diagnosis, prognosis – and ongoing information on disease progression.
The team uses modern genomic techniques to work out why some tumours respond to certain drugs, and others don’t.
“The goal of precision cancer therapy is to get to a time when a cancer patient comes in, has their tumour coded, their immune system coded – and then we choose the appropriate combination of immune regulators that are right for that patient and that tumour,” says Kefford.
“We want to manipulate the immune system in people who are resistant to these drugs today and make their T-cells angry, and force them to attack the tumour.
“The advances now are astonishing and based on data that gets shared all over the world. I'm just a cog in the wheel but proud to be part of a wonderful team.”
Unique resource for trialling tumour treatment
Kefford says that the Melanoma Institute of Australia’s Melanoma Research Database (MRD2) and their BioSpecimen Bank have been key resources for his research.
MRD2 is based on a system of cataloguing patient data that was established in 1968 and now includes the records of melanoma patients including data related to new targeted therapy discoveries, and now contains over 60,000 records.
The Biospecimen Bank extends the data from MRD2 further, and is now the world’s largest collection of melanoma tissue samples, with specimens donated by more than 10,000 patients.
The Institute also runs the Australian Melanoma Genome Project, which is mapping the entire genome of 500 melanomas.
“Macquarie University has contributed generously to the Biospecimen Bank, and it goes beyond blood and tumour samples as a resource, because biospecimens officers have very carefully annotated all those specimens when they were collected,” says Kefford.
Information such as the patient’s treatment history at the time of sample collection, their response to treatment and the drugs they have been given, are all noted along with patient outcomes, he says.
Kefford’s research includes a study published in Nature last year which looked at the genetic differences between melanomas that arise in different parts of the body and other research that explores why and how melanomas in certain patients are resistant to particular classes of drug treatment.
“In our latest work, instead of just taking the tumour samples from patients and freezing them, we are able to dissociate the tumours from the immune cells and then manipulate them in the laboratory,” he says.
These techniques allow the researchers to trial certain drug treatments directly on tumour-affected human cells outside a patient’s body and observe the responses very closely.
“This is an important breakthrough because it's very difficult to model the human immune system in animal models, what happens in mice is not always what happens in people.”
Kefford says that these experiments hope to answer why some patients respond very well to certain treatments but more than half of patients do not.
“We hope to have answers to some of these questions within the next 12 months.”



